Table of Contents
- What is TUDCA?
- What is the recommended TUDCA dosage for Liver Repair?
- How much TUDCA per day should you take?
- What are some potential TUDCA Benefits?
- What are the side effects of a TUDCA Supplement?
- Can TUDCA help with Weight Loss?
- Can TUDCA help with Cancer?
- TUDCA Vs Taurine: What is the difference?
- Is there a relationship between TUDCA and Liver Enzymes?
- Can TUDCA help with Chronic Hepatitis?
- Can TUDCA help with Primary Biliary Cirrhosis?
- What is the TUDCA dose for ALS?
- Can TUDCA help with Insulin Resistance?
- Can TUDCA help with a Liver Transplant?
- Want to know more?
- Sources
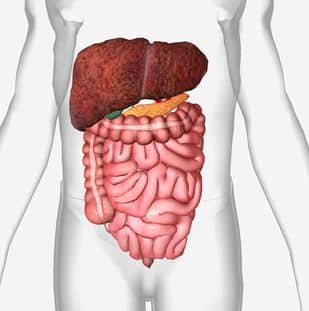
What is TUDCA?
Tauroursodeoxycholic acid (TUDCA) is a a water soluble bile acid, found in naturally in trace amounts in the body.
It is the taurine conjugate form of ursodeoxycholic acid (UDCA)
It has been used as a supplement to treat liver diseases (like cholestasis and cholelithiasis) and overall health (including brain health)
What is the recommended TUDCA dosage for Liver Repair?
According to scientific research, the recommended TUDCA dosage for liver repair is 10-13 mg daily for 3 months, because it seems to stimulate hepatocyte (liver cell) proliferation.
How much TUDCA per day should you take?
For liver health, scientific literature agrees on a dosage range between 500 to 1750 mg daily as a general recommendation of how much TUDCA per day you should take. The list below shows a more detailed breakdown of the dosages for each liver condition:
- Primary biliary cirrhosis: 750 mg daily for 2 months.
- Liver transplant: 500 mg daily for 1 year.
- Chronic hepatitis: 500 to 750 mg daily, for 6 months.
- ALS: 1 g twice daily for 1 year.
- Liver and eye health: two 250 mg capsules daily.
- Primary biliary cholangitis: 250 mg 3 times per day for 24 weeks.
- Bodybuilders: 500 – 1500 mg daily.
- Muscle and liver insulin sensitivity: 1750 mg daily for up to 4 weeks.
- Improving bile salt composition: 15-20 mg per kg of bodyweight.
A wash out period of 3 months is recommended after each 6 month period of ingestion.
In the video below, Dr. Jerry Brainum explains how TUDCA can act as a liver protection supplement.
What are some potential TUDCA Benefits?
TUDCA has potential benefits for liver conditions, some body functions, and some neurodegenerative diseases not related to the liver.
Liver conditions
- Cholelithiasis (gallstones)
- Cholestatic liver disease
- Cholestasis (blockage of liver bile flow)
- Liver Cirrhosis
- Hepatitis
Body functions
- Liver enzymes, mitochondria and cells
- Gallbladder health and bile duct flow
- Insulin sensitivity for diabetes
- Gut microbiome and anti inflammatory
- Cholesterol reduction
- Gene expression
- Protein folding and reduction of stress on the endoplasmic reticulum (ER) of cells
- Brain and eye health
- Heart health
- Kidney health
- Antiviral
Non-liver neurodegenerative diseases
- ALS
- Alzheimer’s disease
- Parkinson’s disease
- Huntington’s disease
- Stroke
This is our recommended TUDCA supplement (Amazon’s Choice):

What are the side effects of a TUDCA Supplement?
The side effects of a TUDCA supplement are gastrointestinal symptoms (diarrhea), itch, rash, and period pain. However, these side effects might only occur if it’s consumed in quantities over 1000 mg daily. Therefore, it’s advised to consume 500 mg daily or less, just to be on the safe side.
UDCA side effects
UDCA (which is similar to TUDCA) showed the following side effects:
Skin issues
- Rash
- Urticaria
- Dry skin
- Worsening of psoriasis
- Hair thinning
Digestive issues
- Bloating
- Nausea
- Constipation
- Stomatitis
- Flatulence
- Biliary pain
- Gallbladder inflammation (cholecystitis)
Mental health issues
- Anxiety
- Depression
- Sleep disorder
Allergies
- Cough
- Allergy
- Rhinitis
Pain and fatigue
- Sweating
- Headache
- Fatigue
- Joint Pain (arthralgia)
- Muscle pain (myalgia)
Can TUDCA help with Weight Loss?
TUDCA might potentially help with weight loss due to the following functions:
- TUDCA may reduce insulin sensitivity, which prevents obesity and helps in weight loss.
- TUDCA has been considered an important regulator of energy metabolism in obesity.
- In a study with mice, TUDCA caused a reduction in fat deposits, which caused weight loss.
Study Title
Glycolipid Metabolism Disorder in the Liver of Obese Mice Is Improved by TUDCA via the Restoration of Defective Hepatic Autophagy
Method used
500 mg/kg of TUDCA was injected into obese mice, and metabolic parameters, autophagy markers, and insulin signaling molecular were assessed.
Results
- The TUDCA injections in the obese mice resulted in a reduced body weight gain, lower blood glucose, and improved insulin sensitivity compared with obese mice that were injected with vehicle.
- Meanwhile, TUDCA treatment not only reversed autophagic dysfunction and endoplasmic reticulum stress, but also improved the impaired insulin signaling in the liver of obese mice.
Conclusions
These results support the hypothesis that TUDCA improves the defective hepatic autophagy, activation of ER stress, and impaired insulin signaling induced by obesity, thereby offering novel opportunities for the treatment of obesity.
Can TUDCA help with Cancer?
Studies suggest that TUDCA can act as healing agent in some types of cancer:
- Liver Cancer: TUDCA reduces liver toxicity caused by liver cancer and prevents tumor formation by decreasing ER stress, inflammation and cell death in cancer tissue.
- Colitis Cancer: TUDCA prevents formation of tumors caused by colitis, hence TUDCA could be a treatment for colitis-associated cancer (CAC).
- Prostate Cancer: TUDCA treatment led to a lower expression of the genes that cause prostate cancer, so TUDCA could potentially help treat prostate cancer.
TUDCA Vs Taurine: What is the difference?
Taurine is an amino acid, and TUDCA is a bile acid produced in the liver, when the bile duct releases bile salts into the large intestine, then microbes metabolize these salts into ursodeoxycholic acid (UDCA), which gets conjugated to Taurine in order to create TUDCA.
For liver function, TUDCA is more powerful than Taurine.
Is there a relationship between TUDCA and Liver Enzymes?
TUDCA has been proven to lower the following liver enzymes associated with liver disease:
- alanine aminotransferase (AST)
- aspartate aminotransferase (ALT)
- alkaline phosphatase (ALP)
- gamma-glutamyl transpeptidase (GGT)
Can TUDCA help with Chronic Hepatitis?
According to a study, TUDCA can improve the biochemical expression of chronic hepatitis. However, more long-term studies are warranted.
Study 1
- Title: Does tauroursodeoxycholic acid (TUDCA) treatment increase hepatocyte proliferation in patients with chronic liver disease?.
- Duration: 3 months.
Subject Information
- Health Status: chronic liver disease.
- Number of subjects: 5.
Despite numerous studies on the effects of bile salts therapy in chronic liver disease, there are no reports on the influence such therapy has on hepatocyte proliferation.
Method used
The aim of this preliminary study was to evaluate the effect of TUDCA on hepatocyte proliferation in 5 patients with HCV-correlated chronic liver disease. All patients were treated with TUDCA (10-13 mg/day) for three months and the determination of PCNA (Proliferating Cell Nuclear Antigen) expression was used to assess the proliferative activity of hepatocytes at the beginning and at the end of treatment.
Results
TUDCA reduced both ALT and Knodell’s score in the 5 patients in whom a significant increase of PCNA-LI was observed after treatment.
Conclusion
TUDCA administration seems to stimulate hepatocyte proliferation in man.
Study 2
- Title: Tauroursodeoxycholic acid for the treatment of HCV-related chronic hepatitis: a multicenter placebo-controlled study.
- Duration: 6 months.
Subject Information
- Health Status: chronic hepatitis.
- Number of subjects: 150.
Method used
One hundred and fifty patients with chronic hepatitis were randomly assigned to receive tauroursodeoxycholic acid at daily doses of 500 mg or 750 mg, or a placebo for 6 months.
Results
A consistent decrease in aminotransferase serum levels was observed in patients treated with tauroursodeoxycholic acid compared with placebo (p<0.001) and a progressive improvement with time was also found (p<0.05; linear time effect).
Conclusions
Tauroursodeoxycholic acid improves the biochemical expression of chronic hepatitis. Long-term studies with clinically relevant end-points are warranted.
Can TUDCA help with Primary Biliary Cirrhosis?
One study concluded that a dose of about 10mg/kg of TUDCA should be used in patients with primary biliary cirrhosis.
Study 1
- Title: Tauroursodeoxycholic acid for treatment of primary biliary cirrhosis. A dose-response study.
- Duration: 6 months.
Subject Information
- Health Status: primary biliary cirrhosis.
- Number of subjects: 24.
Method used
We performed a dose-response study on 24 patients with primary biliary cirrhosis who were randomly assigned to receive 500, 1000, or 1500 mg daily of tauroursodeoxycholic acid for six months.
Results
- Biliary enrichment with ursodeoxycholic acid ranged from 15% to 48% and was not related with the dose.
- Liver enzyme levels decreased significantly after the first month of treatment with all three doses.
- No significant difference among the three doses was found, although further reduction over time occurred with 1000 and 1500mg daily.
- Plasma total and HDL cholesterol significantly decreased in patients administered the two higher doses.
- Diarrhea was the only side effect.
Conclusion
A dose of about 10mg/kg body wt/day of tauroursodeoxycholic acid should be used for long-term studies in patients with primary biliary cirrhosis.
Study 2
- Title: Differences in the metabolism and disposition of ursodeoxycholic acid and of its taurine-conjugated species in patients with primary biliary cirrhosis.
- Duration: 2 months.
Subject Information
- Health Status: primary biliary cirrhosis.
- Number of subjects: 12.
- Gender: female.
The clinical effectiveness of ursodeoxycholate in the treatment of liver disease may be limited by its poor absorption and extensive biotransformation. Because in vitro and in vivo studies suggest that the more hydrophilic bile acid tauroursodeoxycholate has greater beneficial effects than ursodeoxycholate, we have compared for the first time the absorption, metabolism, and clinical responses to these bile acids in patients with primary biliary cirrhosis (PBC).
Method used
Twelve female patients with PBC were administered tauroursodeoxycholate and ursodeoxycholate (750 mg/d for 2 months) in a study. Bile acids were measured in serum, duodenal bile, urine, and feces.
Results
- Biliary ursodeoxycholate enrichment was higher during tauroursodeoxycholate administration (32.6% vs. 29.2% during ursodeoxycholate).
- Lithocholic acid concentration was consistently higher in all biological fluids during ursodeoxycholate administration.
- Fecal bile acid excretion was the major route of elimination of both bile acids; ursodeoxycholate accounted for 8% and 23% of the total fecal bile acids during tauroursodeoxycholate and ursodeoxycholate administration, respectively.
- Tauroursodeoxycholate was better absorbed than ursodeoxycholate, and, although it was partially deconjugated and reconjugated with glycine, it underwent reduced biotransformation to more hydrophobic metabolites.
Conclusion
This comparative study suggests that tauroursodeoxycholate has significant advantages over ursodeoxycholate that may be of benefit for long-term therapy in PBC.
Study 3
- Title: Ursodeoxycholic and tauro-ursodeoxycholic acids for the treatment of primary biliary cirrhosis: a pilot crossover study.
- Duration: 15 months.
Subject Information
- Health Status: primary biliary cirrhosis.
- Number of subjects: 23.
Method used
The effects of ursodeoxycholic and tauro-ursodeoxycholic acids were compared in 23 patients with primary biliary cirrhosis according to a crossover design. Both drugs were administered at the daily dose of 500 mg. in a randomly assigned sequence for two 6-month periods separated by a 3-month wash-out period.
Results
Serum liver enzymes related to cholestasis and cytolysis consistently improved, as compared to baseline values, during the administration of both ursodeoxycholic and tauro-ursodeoxycholic acids, but no significant difference between these two bile acids was found. Both treatments were well tolerated and no patient complained of side effects.
Conclusion
In the short-term, tauro-ursodeoxycholic acid appears to be safe and at least as effective as ursodeoxycholic acid for the treatment of primary biliary cirrhosis.
Study 4
- Title: Efficacy and safety of tauroursodeoxycholic acid in the treatment of liver cirrhosis: a double-blind randomized controlled trial .
- Duration: 6 months.
Subject Information
- Health Status: patients with liver cirrhosis.
- Number of subjects: 23 patients were randomly divided into TUDCA group (12) and UDCA group (11).
Method used
The patients were given TUDCA and UDCA respectively at the daily dose of 750 mg, in a randomly assigned sequence for a 6-month period.
Results
- Albumin levels were significantly increased in both TUDCA and UDCA groups.
- Markers for liver fibrosis were slightly decreased with the difference being not significant in either group.
- Only one patient in TUDCA group had significant relief.
- Both treatments were well tolerated and no patient complained of side effects.
Conclusion
- It is suggested that TUDCA therapy is safe and appears to be more effective than UDCA in the treatment of liver cirrhosis.
- However, both drugs exert no effect on the serum markers for liver fibrosis during 6-month treatment.
What is the TUDCA dose for ALS?
The TUDCA dose for ALS is 1 g twice daily (2g daily) for 54 weeks, and Riluzole 50 mg twice daily (100 mg daily).
Study Info
- Title: Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis.
- Duration: 54 weeks.
Subject Information
- Health Status: ALS.
- Number of subjects: 34.
Method used
Patients under treatment were randomized to placebo or TUDCA and were evaluated after a lead‐in period of 3 months.
Results
- Tauroursodeoxycholic acid was well tolerated; there were no between‐group differences for adverse events.
- The proportion of responders was higher under TUDCA (87%) than under placebo (43%).
Conclusion
This pilot study provides preliminary clinical data indicating that TUDCA is safe and may be effective in ALS.
Can TUDCA help with Insulin Resistance?
One study demonstrated that TUDCA might be an effective approach for treating insulin resistance. However, additional studies are needed.
Study Info
- Title: Tauroursodeoxycholic Acid may improve liver and muscle but not adipose tissue insulin sensitivity in obese men and women.
- Duration: 4 weeks.
Subject Information
- Health Status: obese.
- Number of subjects: 20.
Method used
Patients were randomized to 4 weeks of treatment with TUDCA (1,750 mg/day) or placebo.
Results
- Liver and muscle insulin sensitivity increased by approximately 30% after treatment with TUDCA but did not change after placebo therapy.
- In addition, therapy with TUDCA, but not placebo, increased muscle insulin signaling.
- Markers of stress in muscle or adipose tissue did not change after treatment with either TUDCA or placebo.
Conclusion
This data demonstrates that TUDCA might be an effective pharmacological approach for treating insulin resistance. Additional studies are needed to evaluate the target cells and mechanisms responsible for this effect.
Can TUDCA help with a Liver Transplant?
Research shows that treatment with TUDCA after a liver transplant is safe, however, it has no effect on graft function and survival.
Study Info
- Title: One-year pilot study on tauroursodeoxycholic acid as an adjuvant treatment after liver transplantation.
- Duration: 12 months.
Subject Information
- Health Status: undergoing liver transplantation.
- Number of subjects: 33.
Method used
- Sixteen patients were randomized to receive tauroursodeoxycholic acid (250 b.i.d. for 12 months) and 17 served as controls.
- Tauroursodeoxycholic acid was given from day 5 after transplantation for one year.
Results
- Tauroursodeoxycholic acid treatment was safe and well tolerated.
- No drop outs occurred.
- The one-year actuarial survival was 78.6% in patients treated with tauroursodeoxycholic acid and 86.7% in controls.
- No differences were observed with respect to early or late graft function and survival, nor to acute cellular rejection.
- Tauroursodeoxycholic acid therapy was associated with lower cholesterol levels during the early postoperative months; with milder cholestasis; with a drop in biliary cholates but no changes in bile salts.
Conclusion
Long-term treatment with low dose tauroursodeoxycholic acid after liver transplantation is safe but does not affect graft function and survival.
Want to know more?
Click the links below to access the individual topic pages:
Sources
- Crosignani A, Battezzati PM, Setchell KD, Invernizzi P, Covini G, Zuin M, Podda M. Tauroursodeoxycholic acid for treatment of primary biliary cirrhosis. A dose-response study. Dig Dis Sci. 1996 Apr;41(4):809-15. doi: 10.1007/BF02213140. PMID: 8674405.
- Invernizzi P, Setchell KD, Crosignani A, Battezzati PM, Larghi A, O’Connell NC, Podda M. Differences in the metabolism and disposition of ursodeoxycholic acid and of its taurine-conjugated species in patients with primary biliary cirrhosis. Hepatology. 1999 Feb;29(2):320-7. doi: 10.1002/hep.510290220. PMID: 9918905.
- Crosignani A, Budillon G, Cimino L, Del Vecchio Blanco C, Loguercio C, Ideo G, Raimondo G, Stabilini R, Podda M. Tauroursodeoxycholic acid for the treatment of HCV-related chronic hepatitis: a multicenter placebo-controlled study. Hepatogastroenterology. 1998 Sep-Oct;45(23):1624-9. PMID: 9840118.
- Larghi A, Crosignani A, Battezzati PM, De Valle G, Allocca M, Invernizzi P, Zuin M, Podda M. Ursodeoxycholic and tauro-ursodeoxycholic acids for the treatment of primary biliary cirrhosis: a pilot crossover study. Aliment Pharmacol Ther. 1997 Apr;11(2):409-14. doi: 10.1046/j.1365-2036.1997.124295000.x. PMID: 9146783.
- Panella C, Ierardi E, De Marco MF, Barone M, Guglielmi FW, Polimeno L, Francavilla A. Does tauroursodeoxycholic acid (TUDCA) treatment increase hepatocyte proliferation in patients with chronic liver disease? Ital J Gastroenterol. 1995 Jun;27(5):256-8. PMID: 8541578.
- Pan XL, Zhao L, Li L, Li AH, Ye J, Yang L, Xu KS, Hou XH. Efficacy and safety of tauroursodeoxycholic acid in the treatment of liver cirrhosis: a double-blind randomized controlled trial. J Huazhong Univ Sci Technolog Med Sci. 2013 Apr;33(2):189-194. doi: 10.1007/s11596-013-1095-x. Epub 2013 Apr 17. PMID: 23592128.
- Elia, A E et al. “Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis.” European journal of neurology vol. 23,1 (2016): 45-52. doi:10.1111/ene.12664
- Kars M, Yang L, Gregor MF, Mohammed BS, Pietka TA, Finck BN, Patterson BW, Horton JD, Mittendorfer B, Hotamisligil GS, Klein S. Tauroursodeoxycholic Acid may improve liver and muscle but not adipose tissue insulin sensitivity in obese men and women. Diabetes. 2010 Aug;59(8):1899-905. doi: 10.2337/db10-0308. Epub 2010 Jun 3. PMID: 20522594; PMCID: PMC2911053.
- Angelico M, Tisone G, Baiocchi L, Palmieri G, Pisani F, Negrini S, Anselmo A, Vennarecci G, Casciani CU. One-year pilot study on tauroursodeoxycholic acid as an adjuvant treatment after liver transplantation. Ital J Gastroenterol Hepatol. 1999 Aug-Sep;31(6):462-8. PMID: 10575563.
- Guo Q, Shi Q, Li H, et al. Glycolipid Metabolism Disorder in the Liver of Obese Mice Is Improved by TUDCA via the Restoration of Defective Hepatic Autophagy [retracted in: Int J Endocrinol. 2020 Nov 28;2020:2138532]. Int J Endocrinol. 2015;2015:687938. doi:10.1155/2015/687938
- Kusaczuk M. Tauroursodeoxycholate-Bile Acid with Chaperoning Activity: Molecular and Cellular Effects and Therapeutic Perspectives. Cells. 2019 Nov;8(12). DOI: 10.3390/cells8121471.
- Vandewynckel YP, Laukens D, Devisscher L, et al. Tauroursodeoxycholic acid dampens oncogenic apoptosis induced by endoplasmic reticulum stress during hepatocarcinogen exposure. Oncotarget. 2015;6(29):28011-28025. doi:10.18632/oncotarget.4377
- Kim YH, Kim JH, Kim BG, Lee KL, Kim JW, Koh SJ. Tauroursodeoxycholic acid attenuates colitis-associated colon cancer by inhibiting nuclear factor kappaB signaling. J Gastroenterol Hepatol. 2019 Mar;34(3):544-551. doi: 10.1111/jgh.14526. Epub 2018 Nov 14. PMID: 30378164.
- Tan B, Jia R, Wang G and Yang J: Astragaloside attenuates the progression of prostate cancer cells through endoplasmic reticulum stress pathways. Oncol Lett 16: 3901-3906, 2018
- P. Portincasa, V. Palmieri, F. Doronzo, G. Vendemiale, E. Altomare, C. Sabbà, G. Palasciano, O. Albano, Effect of tauroursodeoxycholic acid on serum liver enzymes and dyspeptic symptoms in patients with chronic active hepatitis.